
#Medicare crossover definition code
Enrollment is automatic for these members
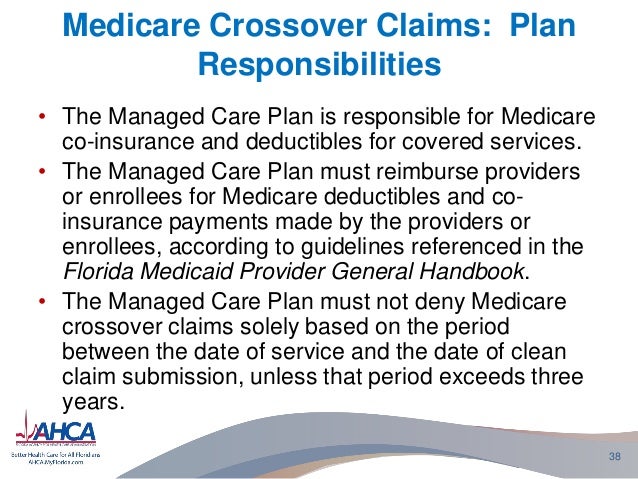
Medicare Crossover is a standard offering for most Medicare-eligible members covered under UnitedHealthcare Commercial plans.Medicare Crossover is the process by which Medicare, as the primary payer, automatically forwards Medicare Part A (hospital) and Part B (medical) including Durable Medical Equipment (DME) claims to a secondary payer for processing.UnitedHealthcare follows 837P/837I guidelines. The service level and claim level should be balanced.
#Medicare crossover definition professional
Preference: Submit professional claims at the line level if primary payer provides institutional claims at either line or claim level.Medicare Acceptance of Assignment: Submit value to indicate whether the provider accepts Medicare assignment.Patient Responsibility Amount: Submit monetary amount the member is responsible for as found on the 835 payment advice or as identified on the Medicare EOB.Medicare Approved Amount: Submit other payer claim level and line level allowed amount when UnitedHealthcare is secondary to Medicare.Medicare Paid Amount: Submit other payer claim level and line level paid amount when UnitedHealthcare is secondary to Medicare.Deductible, co-insurance, copayment, contractual obligations and/or non-covered services are common reasons why the other payer paid less than billed. Do not enter at claim level any amounts included at line level. Adjustment Reason Code: Submit other payer claim adjustment reason code as found on the 835 payment advice or identified on the EOB.Adjustment Group Code: Submit other payer claim adjustment group code as found on the 835 payment advice or identified on the EOB.UnitedHealthcare follows 837P/837I guidelines.ĬOB Electronic Claim Requirements - Medicare Primary Preference: Submit professional claims at the line level and institutional claims at either the line or claim level.Adjustment Amount: Submit other payer adjustment monetary amount.The paid amount on institutional claims can be submitted at the claim level. Primary Payer Paid Amount: Submit the primary paid amount for each service line reported on the 835 payment advice or EOB.COB Electronic Claim Requirements – Commercial


 0 kommentar(er)
0 kommentar(er)
